PERICARDIOCENTESIS
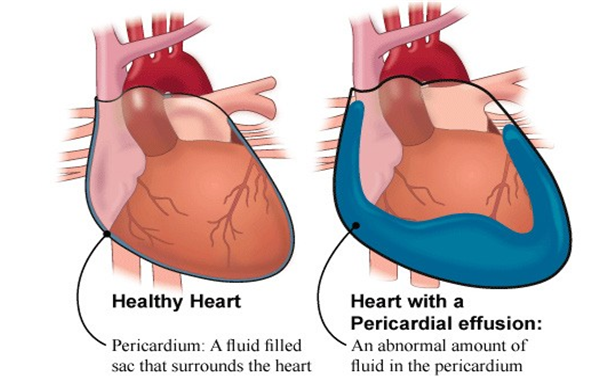
Image Source: Pericardiocentesis_Pericardial_Tap.pdf
What is a Pericardiocentesis (Pericardial Tap)?
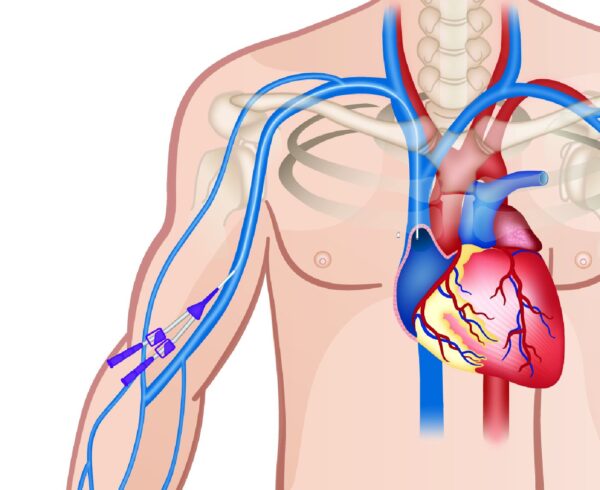
Pericardiocentesis, also called a pericardial tap, is a procedure in which a needle and catheter remove fluid from the pericardium, the sac around your heart. The fluid is removed for either reducing the pressure around the heart and / or to evaluate the disease why this has occurred. It occurs in various diseases which may be either infection, or inflammation, or trauma, or rarely associated with cancers.
Occasionally, pericardiocentesis is done in an emergency to treat something called cardiac tamponade, a life-threatening rapid build-up of fluid around the heart that weakens its pumping. The procedure relieves pressure there.
Why do I need to have this procedure?
The two main aims of the procedure are to:
Relieve symptoms, like shortness of breath, that are caused by the fluid around your heart
Find out if the fluid around your heart is caused by problems such as infection, inflammation, trauma, or cancer.
What can I expect?
Before the pericardiocentesis:
- You usually have a pericardiocentesis in a procedure room or at your bedside. You lie on your back for this procedure, sometimes with a back rest behind your back.
- Your doctor does a special ultrasound of your heart to see how much fluid is around your heart. This helps them decide if you need to have this procedure.
- If you need to have the procedure, your doctor explains it to you and your family and tells you the reasons why a pericardiocentesis is right for you.
- When you are sure you understand why you need the procedure and feel comfortable about having it, they ask you to sign a consent form. This form says you agree to have the procedure.
During the pericardiocentesis:
- We clean the area of your chest just beneath the breast bone with an antiseptic liquid.
- Your doctor numbs (freezes) the area using special medicine. Some patients feel anxious or worried about this procedure. Tell your doctor if you feel anxious and would like medicine to relax you.
- We cover the area with a sterile (very clean) towel, so it is important to keep your hands at your sides.
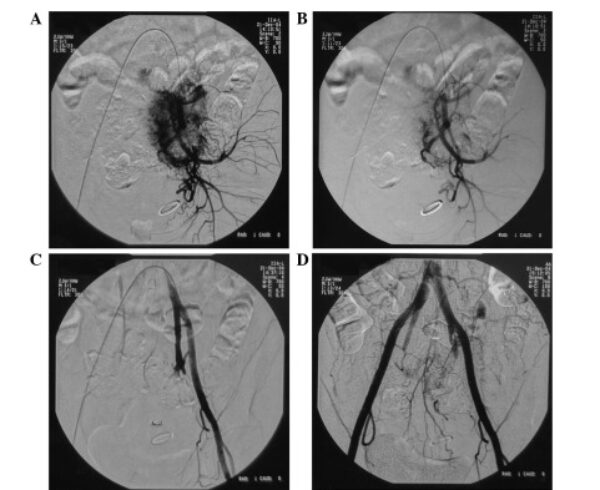
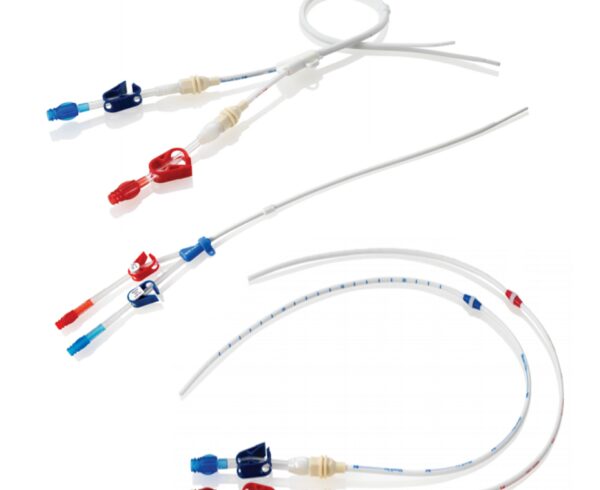
- Your doctor puts a plastic tube (drain) into the area around your heart where the fluid is. You will feel some pressure when the tube is going in, but it should not hurt. If you feel pain, tell your doctor. They can give you more numbing medicine.
- Once the drain is in the right place, your doctor will use a syringe to remove some of the fluid from around your heart
- The fluid is sent samples of the fluid to the laboratory for testing. This will help us find out what caused the fluid to collect around your heart.
- We connect the drain to a collection bag so the remaining fluid can drain slowly. The tube is held in place with stitches, and we place a dressing over the area.
What can I expect after the procedure?
- You should start feeling better once some of the fluid is removed from around your heart.
- The drain is sometimes left in place for 1 or 2 days. You may have pain at the area once the numbing wears off. If you have pain, tell your nurse. They can give you medicine to take the pain away.
- Don’t touch or tug at your dressing or drain. Ask your nurse if you need help when moving in bed. Keep the dressing dry at all times.
- Once the fluid stops draining into the collection bag, your doctor does another ultrasound of your heart to make sure all the fluid is gone.
- If there is no more fluid, your doctor removes the drain and covers the area with a small dressing.
- There will be a tiny hole in your chest area when we take the drain out. This will heal on its own and doesn’t need any sutures.
Based on the reports of the fluid appropriate treatment is given to prevent its recurrence.
What are the risks of pericardiocentesis?
All procedures have some risks. The risks of pericardiocentesis include:
- Puncturing the heart, which may require surgery to repair
- Puncturing the liver
- Excess bleeding, which might compress the heart and affect its normal function
- Air in the chest cavity
- Infection
- Abnormal heart rhythms (which can cause death in rare instances)
- Heart failure with fluid in the lungs (rare)
There is also a chance that the fluid around the heart will come back. If this happens, you might need to repeat the procedure, or you might eventually need all or part of your pericardium removed.
Your own risks may vary according to your age, your general health, and the reason for your procedure or type of surgery you have. They may also vary depending on the anatomy of the heart, fluid, and pericardium. Talk with your healthcare provider to find out what risks may apply to you.






Ask a Question?