INTRODUCTION AND HISTORY
To better understand the present scenario and practices in Critical Care medicine in India, we need to first understand the history and evolution of the specialty over period of time.
The concept of critical care and the understanding of the need for special attention to seriously ill patients started back in 1850s. During Crimean war in early 1850 Florence nightingale demanded most seriously ill patients be kept near the nursing station. She realized, those patients needed close monitoring and early treatment. After this, it took many years to make any substantial progress in this field. In year 1923, a 3 bedded ICU was set up in John Hopkins Hospital in Baltimore USA, to take care of post-operative neurosurgical patients. In the next decade many other hospitals followed the suit and post-operative surgical care units to take care of postoperative patients.
Image Source: https://nursekey.com/florence-nightingale-where-most-work-is-wanted
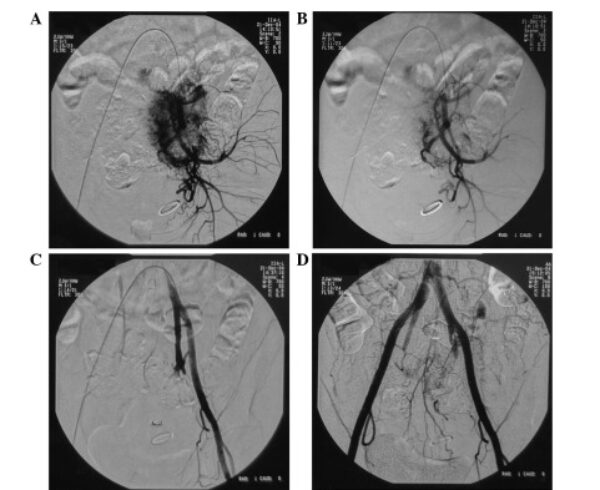
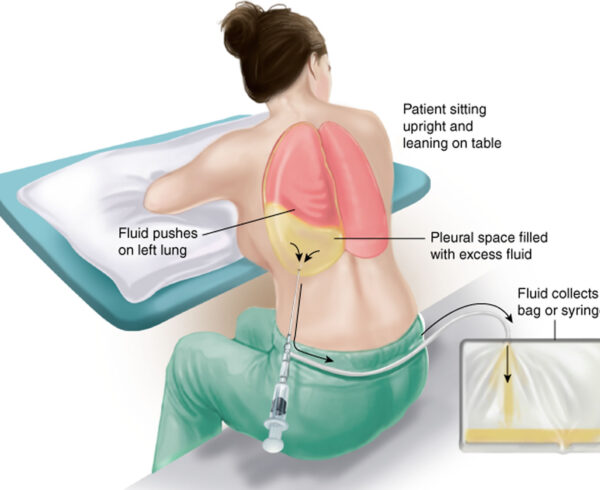
The most significant event leading to beginning of modern Critical Care was the Copenhagen polio epidemic in 1952. These polio patients used to have muscle weakness manifesting as respiratory failure and pooling of secretions. Ultimately they used to succumb. Rate of death of such patients was approximately 80 to 90 percent of total cases. At this time to assist the breathing of such patients only 7 respirators were available – 1 tank respirator and 6 cuirass respirators. It was impossible to manage such a high load of critical patients needing ventilator support. So Medical and Dental students were deployed to use hand ventilators and ventilate such patients manually by giving assisted breaths. Every week around 300 patients were given assisted manual respiration support during this time. The mortality rate came down to around 40% and the world realized the importance of special attention to such patients. In 1953 modern ICU was set up in Europe doctor Bjorn Isberg, who is now considered as the father of modern Critical Care medicine.
Cuirass Respirator

Image Source: http://museum.aarc.org/gallery/negp
Iron Lung

Image Source: https://en.wikipedia.org/wiki/Iron_lung
In early 1960 Max Harry well started ‘shock beds’ in Los Angeles where he would admit patients with low blood pressure.
Over time it was realized that senior experienced doctors could not be at the bedside for the whole day so over period of next few years Junior Doctors were appointed for continuous care of such patient and eventually shift duties with staff around the clock became the routine practice in ICUs.
The first microprocessor controlled ventilator was introduced in 1971. As the technology progressed with advent of new equipment and new drugs, life support systems became compact and more accurate. Dedicated ICU nurses, physiotherapists, pharmacists, dietitians, technicians, microbiologists, radiologists, infectious disease specialist etc. started manning the ICUs and further improved the quality of Intensive Care.
After 1990 the ‘evidence based medicine’ started picking up. All the practices changed gradually based on the current best evidence. Quality of research improved. Multicenter trials became reality. We became wiser in treating critical patients.
Coming to the Indian scenario, in early 1970 is some of the major hospitals started with ‘coronary care units’ to take care of patience with ‘heart attacks’. In mid 1970s Dr Farokh E Udwadia set up for the first time in India, respiratory Care Units in Mumbai. These respiratory care units helped reduce mortality cases of tetanus.
In those times, doctors having keen interest in the branch of critical care medicine used to go abroad and take training. Some of these enthusiastic doctors came back to India and started practicing Critical Care medicine. Eventually, the Indian society of Critical Care medicine (ISCCM) was formed in 1992. After The formation of ISCCM, regular conferences workshops and continuing medical education programs started happening in India. Postdoctoral training programs fellowships started. Number of scientific publications in the subject of Critical Care medicine from India also started coming up.
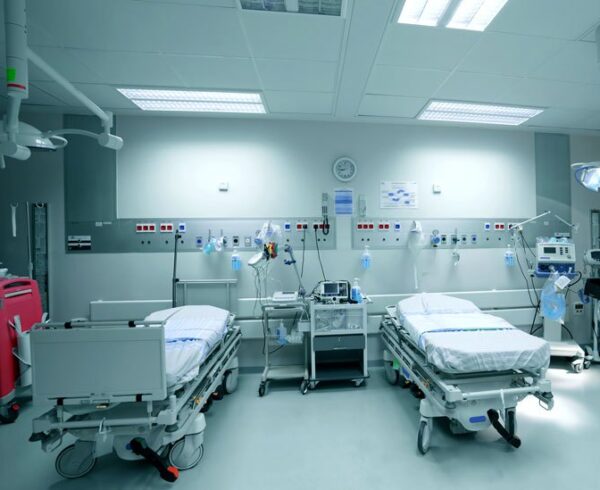
In an early ICU, patients felt isolated and the attendants felt a sense of mystery about ICU. At that time, strict isolation protocols were followed for all patients, gowns masks, shoe covers etc were used extensively Supramaximal goals were the norm. As evidence based medicine evolved and we got more research based results, the image of ICU has changed. In the current scenario use of the advanced technology and sophisticated machines – which are portable, compact, more accurate and simultaneously less invasive – have led to complete makeover of the old image of ICUs. We now understand the benefits of contact of patients with their loved ones. Presently, the visiting policy has become more liberal, there is better communication with patients and families. Today ‘Less is More’ is the norm. Our targets for oxygenation, blood pressure, tidal volume etc. have become less aggressive. Our transfusion thresholds and resuscitation thresholds have become more restricted.
Changing place of the ICU within the hospital
As compared to earlier scenario where ICU would occupy only 3 to 5% of beds of the whole Hospital the new hospitals have 10 – 15 % of their beds allotted for the critical care facilities. This change has happened because of better understanding of medicine and better recognition of Intensive Care/Critical care Medicine as a superspeciality. This number may become even higher in future.
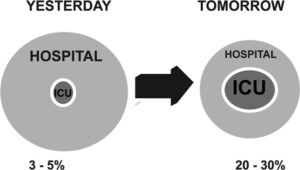
Image Source: https://www.researchgate.net/figure/Changing-place-of-the-ICU-within-the-hospital-Schematic-to-demonstrate-the-increasingly_fig1_236066378
Type of ICUs in India
Critical care in India is generally provided by three types of hospitals.
Community hospitals and Medical College associated hospitals
These hospitals are generally funded by the government. The charges for the services and treatment are born by government. Patients do not need to pay for the Intensive Care Services. As these services are expensive, quality of services at such hospitals is not up to the mark. The number of cases covered by these hospitals are also very less.
Private tertiary care hospitals
These hospitals are run by societies trust and companies. Patients are levied charges for the Intensive Care Services. Small percentage of beds are free for poor and low income patients. Usually the ICUs in such hospitals are well equipped. These hospitals form major contribution to Critical Care facilities in our country albeit at a higher cost to patient.
Small hospitals and nursing homes
These facilities are generally run by professionals themselves. They have modest equipments and staffing. Critical Care Medicine, as a branch is coming up rapidly in this sector.





Ask a Question?