COLLAPSED LUNG
Lung collapse is described as any cause that prevents the lung from expanding or let it remain expanded.

Image Source: https://medlineplus.gov/collapsedlung.html
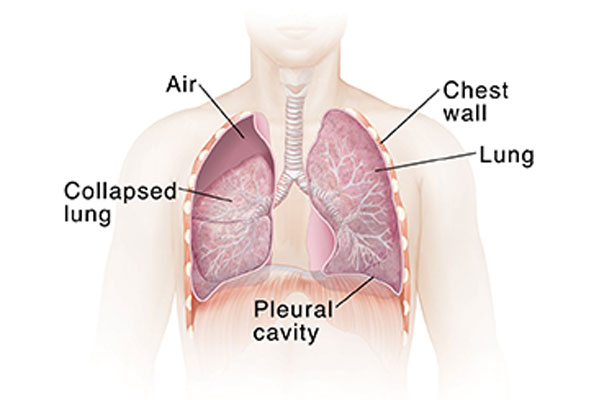
Image Source: https://www.fairview.org/patient-education/85307
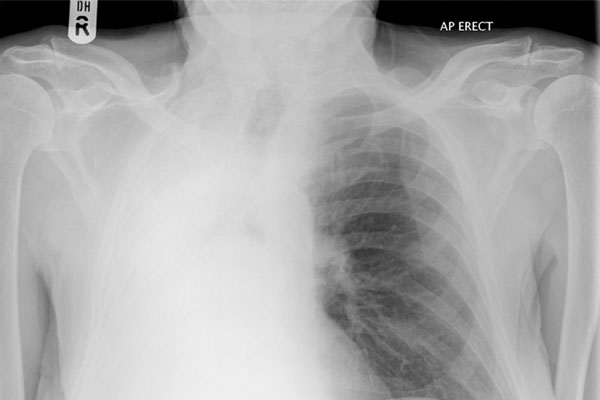
Image Source: https://radiopaedia.org/cases/hemithorax-white-out-lung-collapse
There are multiple reasons that could account for this
Pneumothorax – when air escapes from the lung. The air then fills the space outside of the lung, between the lung and chest wall. This build-up of air puts pressure on the lung, so it cannot expand as much as it normally does when you take a breath.
Mucus plugging – when the patient has an infection in the chest and is unable to cough out or expectorate the phlegm or sputum, the sputum can build up in the airways of the patient leading to loss of air supply or ventilation for the patient and hence collapse of the lung.
Pleural effusion – when there is fluid such as pleural fluid or blood or pus accumulation in the lining of the lungs, it eventually compresses the lung causing collapse.
The management is different in all three scenarios
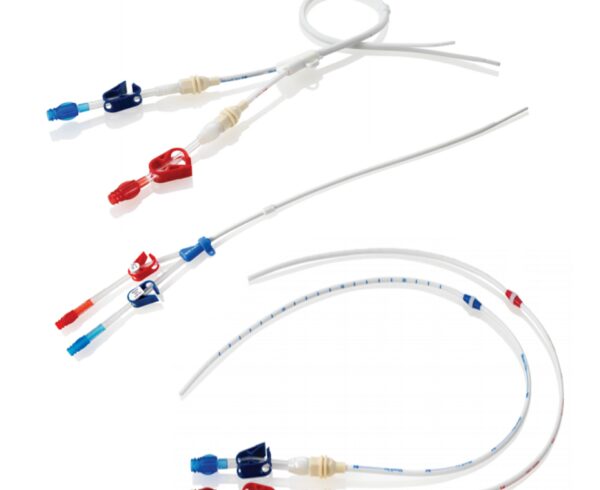
Pneumothorax – this can be a medical emergency, especially if the patient is on a ventilator. A needle or a small tube needs to be inserted into the chest wall up to the lining of the lung to let the air out.
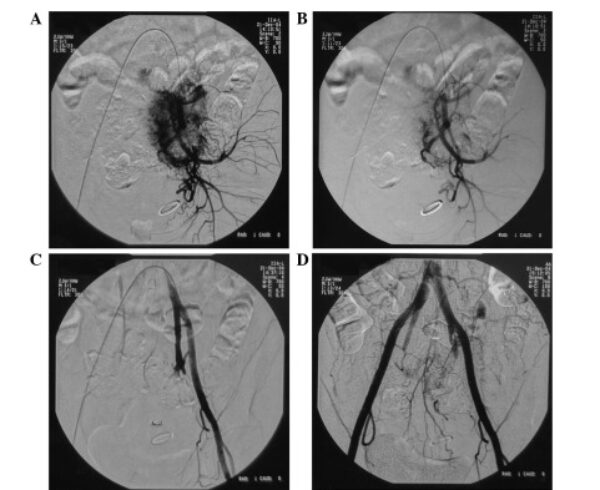
Mucus plugging – good physiotherapy along with nebulisation and mucus thining agents generally are sufficient. However, there may be instances where this is not sufficient, in which case, the doctor may need to do a bronchoscopy ( a small camera is inserted into the lungs through the mouth or nose) and mucus can be suctioned out through the scope.
Pleural effusion – the management is similar to that of pneumothorax.






Hi, I wanted to ask when doctors can remove ventilator. My relative is on ventilator since 7 days and doctors saying he is a case of weaning failure. He had a stroke in brain stem and unconscious. Is tracheostomy mandatory in such cases?
hi…
Mr. Thaker..
At the outset Doctor must have put the ventilator to support the breathing and tracheal toileting. Since the patient is still unconscious and he has suffered brain stem stroke. In such case he will need prolonged ventilatory support and tracheal toileting for which he will need tracheostomy. On the tracheostomy, it will be easy to remove ventilator if patient has good breathing efforts and chances of infection are also less.
Any patient who needs prolonged ventilation should be consider for early tracheostomy for faster recovery.