STROKE PAMPHELET
A stroke is a sudden event that occurs resulting due to death of cells in the brain and results in any of the following symptoms. In common terms stroke is a paralysis attack.
Symptoms of stroke are:
Sudden numbness or weakness of the face, arm or leg (especially on one side of the body)
Sudden confusion, trouble speaking or understanding speech, swallowing.
Sudden trouble seeing in one or both eyes
Sudden trouble walking, dizziness, loss of balance or coordination
Sudden severe most headache ever
Video Source: https://4rai.com/blog/these-3-imaging-tests-can-help-determine-your-risk-of-stroke
A stroke may occur during wakeful hours or it may occur overnight in one’s sleep and get noticed first thing when the person wakes up.
It must be considered as an emergency and no time should be wasted before bringing patient to the hospital.
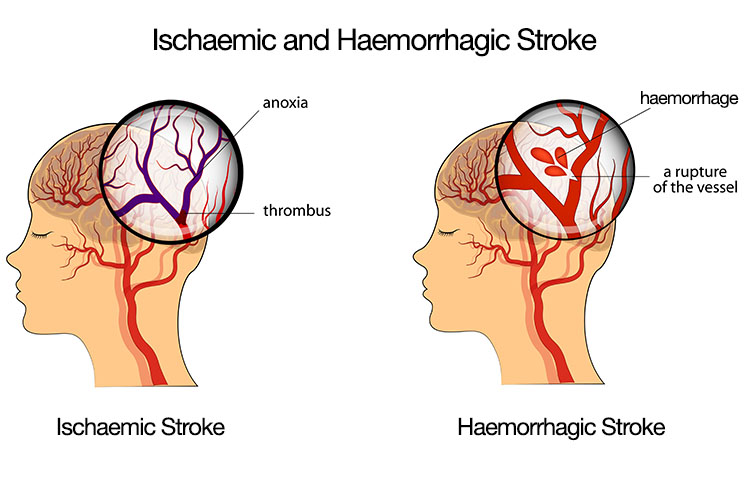
Image Source: https://www.ausmed.com/cpd/articles/different-types-of-strokes
What causes it?
A stroke may be caused by 2 main cause- either due to an infarct (blood clot) or a hemmorage (bleeding in brain). It is not possible however to decide if any particular patient’s stroke is due to an infarct or hemmorage and hence the first step before starting any treatment is a brain scan ( CT scan or MRI).
Basic Anatomy
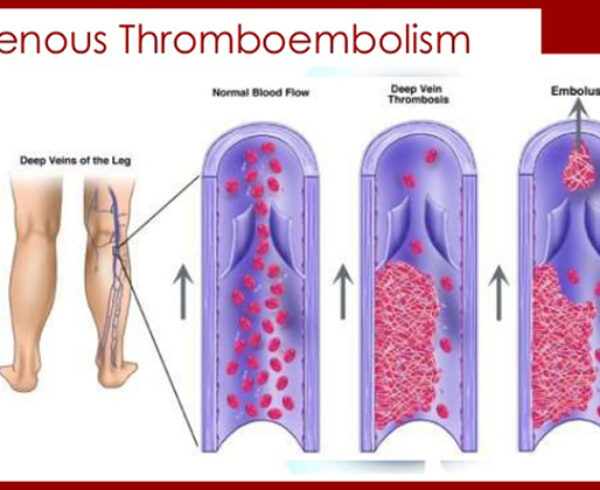
In the simplest way to explain, our brain is supplied by 4 large arteries (1 each to the front part of each side, 1 each to the back part of each side). These 4 further have branching arteries much like a tree progressively becoming smaller and smaller. A blood clot block either the main or any of the brances will lead to a cut off of the blood supply to that area of the brain and hence leading to death of that part of brain. This clot can develop within any of these arteries or can be formed in the heart and travel to the artery and block it.
On the other hand a bleed in any of these blood vessels rupturing either due to high blood pressure or due to rupture of an aneurysm ( a pre-existing weak balloon like structure n the vessel wall)
Risk Factors for having a Stroke
Many people with stroke have other problems or conditions which put them at higher risk for stroke, such as high blood pressure (hypertension), heart disease, smoking, or diabetes.
Not taking Hypertension medicines happens to be a very common cause.
What are the risk factors of stroke?
Hypertension
Diabetes
High cholesterol (presence of excess lipids in the blood)
Smoking
Obesity
Sedentary life style
Lack of excersize
Atrial fibrillation (abnormal and irregular heart rhythm that can alter the heart’s electrical system, resulting in poor blood flow to the body, shortness of breath and weakness)
Family history of stroke
Heavy or binge drinking
Use of illicit drugs such as cocaine and methamphetamines
Cardiovascular disease, including heart failure, heart defects, heart infection or abnormal heart rhythm
Personal or family history of stroke, heart attack or transient ischemic attack

Image Source: https://sera.sg/en/index.php/topic/stroke/stroke_and_risk_factors-01
Other factors associated with a higher risk of stroke include:
Age – People aged 55 years or older have a higher risk of stroke than do younger people.
Race – African-Americans have a higher risk of stroke than do people of other races.
Sex – Men have a higher risk of stroke than women. Women are usually older when they have strokes, and they are more likely to die of strokes than are men.
Hormones – use of birth control pills or hormone therapies that include estrogen, as well as increased estrogen levels from pregnancy and childbirth.

Image Source: https://www.memorialcare.org/services/stroke-care/stroke-prevention
Treatment
The treatment that your doctor can offer depends on two main factors
Is this paralytic stroke due to a infarct (clot) or a bleed.
The time frame within which the patient is brought to hospital.
NOTE: The famous clot busting Injection (Thrombolytic agent) can only be used in stroke due to a infarct (clot) and it can be used only if this is detected within 4.5 hours from onset of symptoms. Also this injection can be given only if the patient does not have any of the following contra-indications.
Initial management in the emergency department
ABC (Airway breathing circulation)
Temperature, Pulse, Blood pressure, Respiratory rate, Oxygen saturation
Sugar level
Collect blood samples for tests
Securing IV lines
ECG
History and Physical examination
Review of patients previous detailed history, ongoing medication list
Any other relevant tests/procedures as may be needed
Next the patient should be shifted for a scan
CT v/s MRI – Which One?
MRI is more sensitive than a CT scan in picking up a small stroke. Also MRI can pick up early strokes (30 min old) which a CT scan often misses. Hence, MRI is ideal.
However, MRI is not available at all hospitals, is more expensive and also more time consuming than CT scan.
Hence, the decision whether to do a CT or MRI rests with your Doctor depending on what is best for the particular patient.
| Time Frame | Treatments |
|---|---|
| Upto 4.5 hrs | Once the Doctor has ruled out any contra-indications to Thrombolysis ( clot-busting therapy), the doctor will explain the benefits and possible risks/dangers of this medicine [Refer table…………] . This medicine will be administered as an Intravenous injection over 1 hour in the ICU setting. Subsequently the patient will be monitored in the ICU over the next few days and a CT/MRI scan will be repeated as needed. Also the patient will later be started on blood thinners.
During this entire period patient will receive Statins( cholesterol medicines), Blood pressure medicines if and as needed. In addition, sometimes if it is large clot blocking one of the large arteries or its initial large branch, an additional procedure called brain angiography and thrombectomy ( clot removal)may be needed. |
| 4.5 upto 16 hours | As the patient is outside the golden window period of 4.5hrs Clot buster cannot be given. Hence , 2 treatments are possible. If a large clot is seen on CT/MRI scan a thrombectomy (clot removal) can be attempted.
If no large clot then blood thinners would be started and patient observed in an ICU setting and other supportive care given |
| > 16 hrs | As patient is outside the time frame for both Clot buster agent and thrombectomy ( clot removal), the doctor will start blood thinners and statins (cholesterol medicines) and observe patient in ICU |
Note: Despite above treatments a possibility of another clot occurring exists and this risk is highest in the first 2-3 days and hence the need for close observation
Benfits & Risks of Thrombolysis
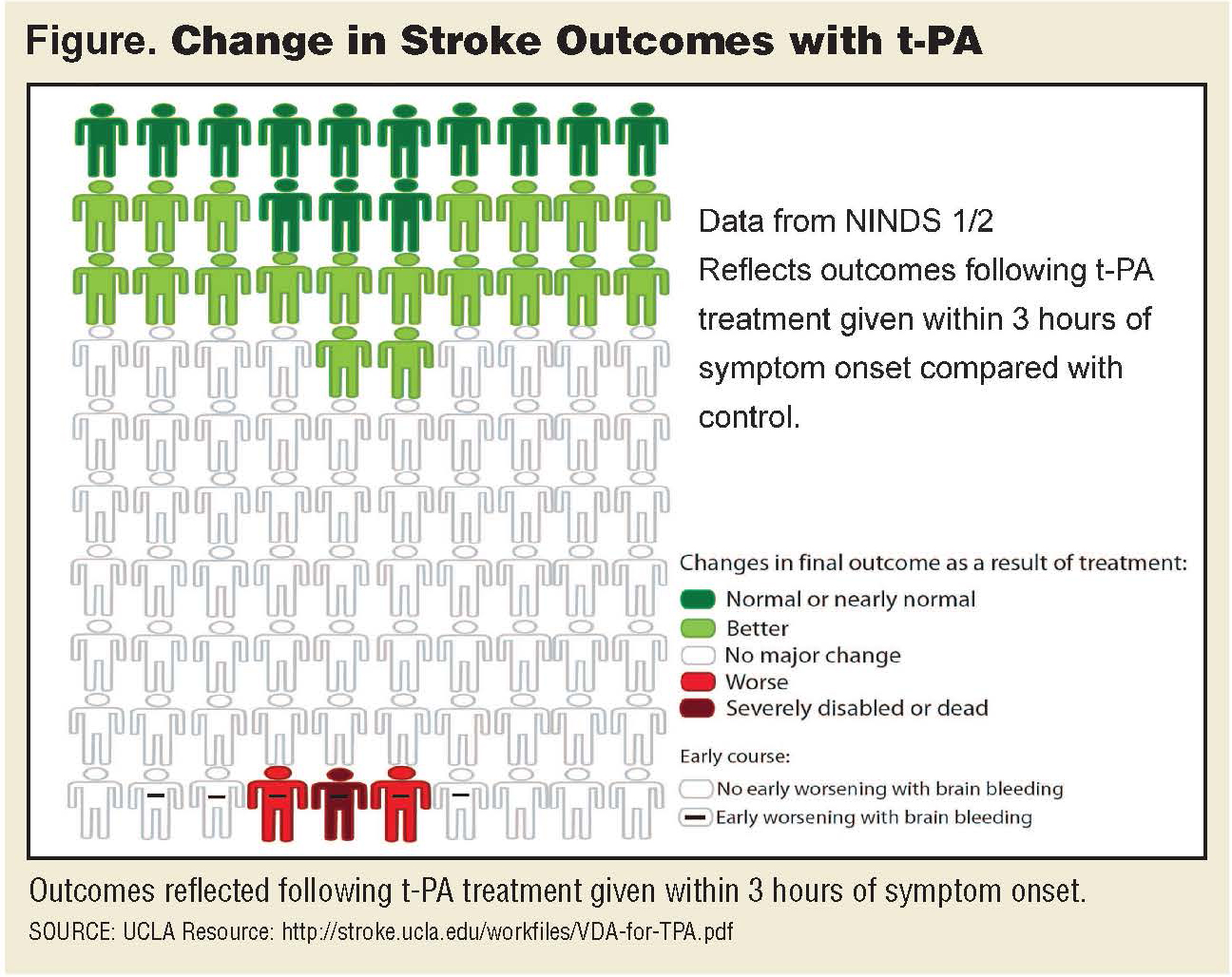
Image Source: http://oc1dean.blogspot.com/2015/08/change-in-stroke-outcome-with-tpa.html
The benefit of thrombolysis is improved blood flow through opening up of the occluded blood vessels and restoring blood supply to affected parts of the brain. This way we can salvage some brain tissue from being further damaged and involved.
However one must understand that the chief benefit of thrombolysis is improved final functional outcome and not immediate relief of symptoms. That means we will not see a sudden improvement in the patient’s stroke symptoms but rather it is the final outcome over the next few months that is expected to be better than if we would not have thrombolysed.
The chief risk is intracerebral hemorrhage i.e. bleeding in the brain.
With intravenous thrombolysis, about 6% of patients have intracerebral hemorrhage associated with early worsening, and half of these patients have their final outcome altered as a result. Other less frequent complications of thrombolysis include Bleeding from elsewhere in the body, and allergic reactions to this medicine.
The figure below is a commonly depicted figure to show the benefits and risks of intravenous thrombolytic therapy provided to patients. It shows that on an average, of every 100 patients treated, 32 will have a better final outcome and 3 will have a worse final outcome ( including sudden death due to massive brain hemmorage) and remaining 65 have an unchanged final outcome if they are thrombolysed or not.
TREATMENT IN CASE OF HEMMORAGE
In case of Hemorrhage, there is no specific medication as such.
Patient would be admitted to ICU and control of ABC (airway breathing circulation), Blood pressure management, close observation done. If needed scans would be repeated. Some patients may require emergency surgery to evacuate the bleed in the brain. The benefits and risks of these would be explained in detail by your doctor before getting consent to go ahead with this procedure. It is important to note that in serious cases this surgery may be just life-saving and may still not improve the patients stroke or the patients comatose state.
Transient Ischaemic Attack (TIA)
A transient ischemic attack (TIA is a temporary, short-lasting stroke. The symptoms are similar to those in a stroke. It may last for just a few seconds or upto hours.
Like an ischemic stroke, a TIA occurs when a clot or debris blocks blood flow to part of your nervous system — but there is no permanent tissue damage and no lasting symptoms. However, it is of utmost importance to understand that this TIA is warning sign that another larger stroke may be coming soon. Hence, never ignore the symptoms of a TIA and seek emergency care even if your symptoms seem to clear up. The management will include admitting the patient and investigating completely for a cause. The risk of second TIA/larger stroke is maximum in the initial few days but persists for months and hence the need to start treatment with blood thinners and cholesterol medications as required.
The risk factors for a TIA are the same as that for a stroke.
Having a TIA puts you at greater risk of having a full-blown stroke, causing permanent damage later. If you’ve had a TIA, it means there’s likely a partially blocked or narrowed artery leading to your brain or a clot source in the heart.
Future Prevention
Identifying the cause of the stroke can help formulate a plan for prevention of future similar events. Also identifying stroke risk factors and following your doctor’s recommendations and adopting a healthy lifestyle are the best steps you can take to prevent a stroke. If you’ve had a stroke or a transient ischemic attack (TIA), it is a wake up call to very strictly follow the life style changes as advised.
Many stroke prevention strategies are the same as strategies to prevent heart disease. In general, healthy lifestyle recommendations include:
Taking medications on time.
Healthy diet advice
Quitting tobacco use.
Controlling diabetes.
Maintaining a healthy weight.
Eating a diet rich in fruits and vegetables.
Exercising regularly.
Drinking alcohol in moderation, if at all.
Treating obstructive sleep apnea (OSA).
Avoiding illegal drugs.
FAQ's
Dr. will this brain clot dissolve?
Per se the clot in the blood vessel would dissolve but the part of the brain damaged ( the affected area on a CT/MRI scan) can never recover. However, the patient can regain his strength over time.
Then Dr. if that dead part cant recover how will my patient improve?
The surrounding part of the brain can take over the function of the dead part and hence do double work. However, this may not happen if there is a very large stroke. Also the ability of the surrounding brain to do this double work depends on how much we can stimulate the patient to use the weakened parts of the body by doing physiotherapy, music therapy, speech therapy and involving the patient in other mental games and hobbies as a part of overall motivation.
Is physiotherapy important or are medicines enough?
Physiotherapy is the cornerstone for recovery of weak limb. It is not only required for regaining strength in a weak limb in the long term but also to prevent joint contractures/ frozen shoulder etc in the short term. It must continue for a long time and must be performed atleast 2-3 times or more daily.


Ask a Question?