GUIDE ON PRESSURE ULCER
Pressure Ulcers – A Guide for patient and caregivers
PRESSURE ULCER
Pressure ulcers may also be called bed sores or pressure sores or pressure injury Skin reddening that disappears after pressure is removed is normal and not a pressure ulcer.
What is a pressure ulcer?
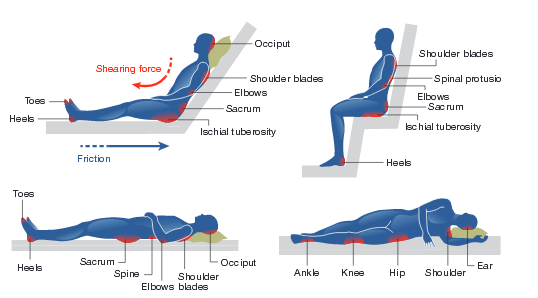
A pressure ulcer is damage that occurs on the skin and underlying tissue. Pressure ulcers are caused by three main things:
Shear – the layers of the skin are forced to slide over one another or over deeper tissues, for example when you slide down or are pulled up, a bed chair or when you are transferring to and from your wheelchair, blood vessels can stretch or bend and can cause pressure ulcer
Friction – rubbing the skin
Or combination of all the above
Moisture – Extra moisture frequently on skin
Where can pressure ulcers develop???
The most common places for pressure ulcers to develop are over bony prominences (bones close to the skin).
Risk Factors
Being unable to move
Loss of bowel or bladder control
Poor nutrition -if you cannot eat a balanced diet, your skin may not be properly nourished.
Pressure ulcers are more likely to form when skin is not healthy.
Are seriously ill or undergoing surgery
Have had pressure ulcers in the past
Lowered mental awareness
Persons who are in a coma or who are paralyzed or who have a hip fracture are at special risk.
Risk Factors in Critical Area
Decreased tissue perfusion due to pressure on the skin
Body temperature
Low immunity
Infection
Low albumin level
Malnourished or undernourishment
Restricted mobility
Damaged sensory perceptions
Incontinence is a common and difficult problem
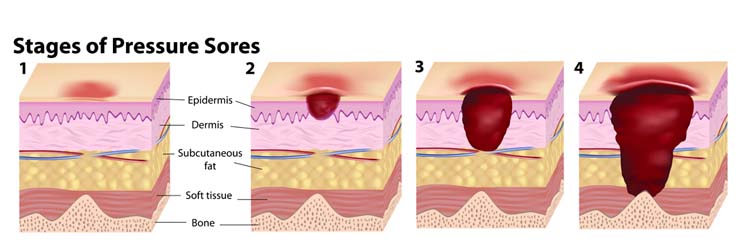
Grades of Pressure Ulcer

Stage: I
Intact skin with non – blanchable redness of a localized area usually over a bony prominence.

Stage: II
Partial thickness loss of dermis presenting as a shallow open ulcer with a red pink wound bed, without slough.
Stage: III
Full thickness loss. Subcutaneous fat may be visible but bone, tendon or muscles are not exposed. Slough may be present.
Stage: IV
Full thickness tissue loss with exposed tendon or muscle. Slough or eschar may be present.

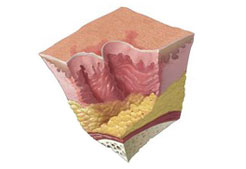
Deep Tissue Injury
Purple or maroon localized area of discolored intact skin or blood – filled blister due to damage of underlying soft from pressure and/ or shear.

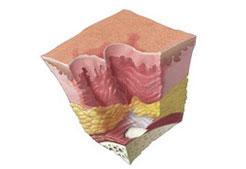
Unstageable
Full thickness tissue loss in which the base of the ulcer is covered by (yellow, tan, gray, green or brown) and/ or eschar (tan brown or black) in the wound bed.

Care Bundle in Critical Care
Risk Assessment to plan the care as per Braden scale risk
Skin Assessment on admission and in each shift/ whenever positioning to keep skin clean and soft healthy
Support Surface i.e. pressure relieving mattress wrinkle free linen, off loading dressings on bony prominence
Nutrition as per body requirement
Repositioning as per patients need
Managing moisture via incontinence care, catheter ,skin barrier spray
Key Factors to Prevent
Position- Should be changed every 2 hourly with left and right lateral
with supine position
Avoid lying directly on your hip bone (trochanter) when lying on your side.
When the head of the bed is raised more than 30 degrees, damaging skin and tiny blood vessels.
Also, a position that spreads weight and pressure more evenly should be chosen – pillows may also help.
Pillows or wedges should be used to keep knees Or ankles from touching each other.
If you are completely immobile, pillows should be put under your legs from mid-calf to ankle to keep heels off the bed.
Avoid placing pillows behind the knees.

IAD (Incontinence associated dermatitis)
If patient is having incontinence (poor control on bladder or bowel) may lead to Diaper rash in medical term it is known as IAD (Incontinence Associated Dermatitis). If we do not take care of IAD it may lead to pressure ulcer.

DIFFERENCE BETWEEN IAD & PRESSURE ULCER
IAD
IAD can occur whenever urine/stool comes in contact with the skin
With IAD affected skin is red or bright red
Blanchable or non blanchable erythema pink or white surrounding skin due to maceration
Skin damage pattern is diffuse
Irregular & asymmetrical shape
Over a fatty parts of the buttocks & thigh, groin
The depth of IAD related skin damage usually is partial thickness without necrotic tissue or slough
PRESSURE ULCER
Arises on bony prominences in the absence of moisture due to pressure, shear & friction
Skin may take on a red, bluish, yellow or Black in colour
Nonblanchable erythema is a grade 1 pressure ulcer
With a pressure ulcer edges are distinct
Will be circular & symmetrical shape
Over a bony prominences
Skin damage depth may vary, necrotic tissue with slough may present



Ask a Question?